Brain Function Monitoring – Clinical Applications
A More Complete Picture Starts with More Complete Data
Home / Clinical Applications
Clinical Applications

Anaesthesia
Anaesthesia
A More Complete Picture of the Brain's Response to Anaesthesia
Brain function monitoring delivers clear, objective, real-time insight into a patient's depth of anaesthesia and sedation. To facilitate faster assessment of patient status, the SedLine monitor provides the Patient State Index (PSi™), a calculated measure of brain activity that reflects the patient's current level of sedation/anaesthesia1. Visit the Technology section to learn more about how the PSi is calculated.
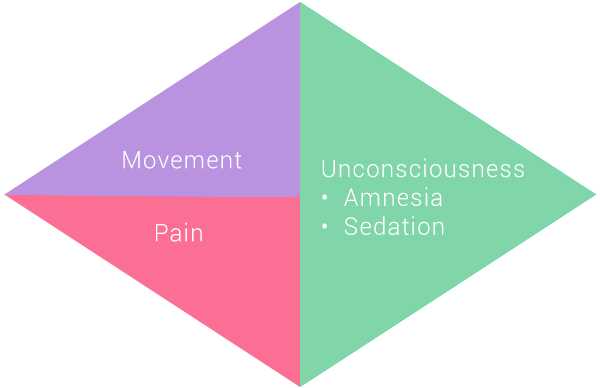
The goal of anaesthesia during a surgical procedure—for an event-free case—is to administer a balance of drugs that achieve appropriate levels of:
- Areflexia (absence of movement)
- Analgesia (absence of pain)
- Loss of consciousness (sedation/hypnosis)
When used as an adjunct to traditional monitoring, brain function monitoring enables the anaesthesia provider to deliver the desired level of targeted sedation throughout all phases of anaesthesia to:
- Optimise anaesthetic depth
- Enhance patient care
Geriatric patients
- Variable response to anaesthetics
- Minimum alveolar concentration (MAC) of inhalation agents decreases with age
- For every 10-year age increase, 6% decrease in MAC
- Increased sensitivity to opioids
- More susceptible to overdose and slow recovery in post-anaesthesia care unit (PACU)
- Changes in haemodynamics have little to do with anaesthetic depth; a more accurate reflection of patient's baseline physiological status
- Brain function monitors help titrate anaesthetic to keep patient in optimum range
- Allows anaesthesiologists to control changes in BP with vasoactive drugs rather than extra anaesthetic
- Facilitates reduced use of anaesthetics which may influence POCD (Post operative cognitive dysfunction
- Brain function monitoring enables fast extubation

"I have found that as I have used depth of anaesthesia monitoring in the operating room that the majority of the changes in hemodynamics that occur in the elderly patient during the surgical procedures have very little to do with the amount of anaesthesia they are getting."
- Terri Monk, MD
- Professor
- Department of Anaesthesiology
- Duke University Medical Center
- Durham, NC

"SedLine gives me a better idea of where I stand at each phase of anaesthesia. The brain number helps guide me to make subtle changes in my anaesthetic appropriate for the patient's heart rate and blood pressure, and thus arrive at the end where I want to be."
- David Drover, MD
- Associate Professor of Anaesthesia
- Stanford University Hospital
- Stanford, CA
Morbidly obese patients
- Difficult to intubate and secure patient's airway
- Drugs distributed differently
- Fat layers store anaesthesia and can result in over- or under-anaesthetizing patient
- Postoperatively, patients recover differently from anaesthesia
- Brain function monitors should be used throughout anaesthetic process to help better judge amount of induction agent
- During maintenance phase, brain function monitoring facilitates individualised titration and can minimise amount of anaesthesia administered

"Adequate monitoring and the use of SedLine and cerebral function monitoring, I believe, is important in these patients. It should be started before we begin the anaesthetic and then utilized throughout the time that one does so."
- Martin Allard, MD
- Professor of Anaesthesiology
- Dir. of anaesthesia Research
- Loma Linda University Medical Center
- Loma Linda, CA
Ventilated ICU patients
- Still struggling to properly sedate ventilated patients in the ICU
- Most patients are over-sedated, resulting in increased time spent on ventilation with a prolonged stay in the ICU and increased costs
- Goal is to more tightly control sedation to avoid these negative outcomes
- Brain function monitoring is a functional tool in the ICU that may help to reduce:
- Costs
- Morbidity
- Length of stay in the ICU

"We need much better monitors of the brain and to use these monitors of the brain. I think this is the advantage that SedLine brings to you is that it doesn't just look at one little area of the brain. It looks at both sides of the brain."
- Michael Ramsay, MD
- Chairman
- Department of Anaesthesiology
- Baylor University Medical Center
- Dallas, TX
ICU Sedation
ICU Sedation
Accurately assessing level of sedation in ICU patients has been a challenge. The effectiveness of using physiologic measures such as vital signs or response to stimulation is compromised by the presence of other drugs. Monitoring sedation through the use of sedation assessment scales is limited to single point measures in time. Further, the accuracy of sedation assessment scales may be compromised by subjectivity and inter-rater variability.
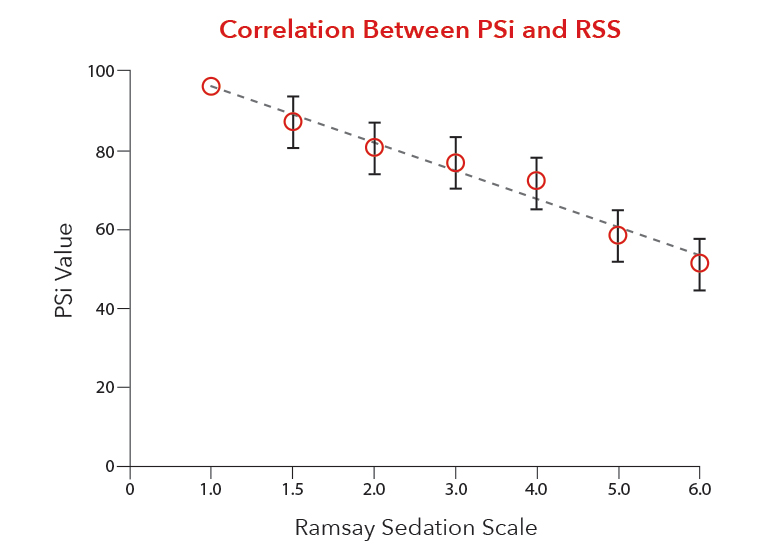
Correlation Between PSi and Ramsay Sedation Scale (RSS)
A strong correlation between the PSi values and the Ramsay Sedation Scale (RSS) as demonstrated in a recent study2 provides the opportunity to effectively manage sedation and analgesia in an objective, consistent manner across the continuum of care, especially in intubated, ventilated ICU patients. Further, changes in the PSi in response to clinical events provide an early warning for patient safety as highlighted in a recent review of sedation measures in the ICU3.
By enabling a more accurate assessment of a patient's level of sedation, SedLine helps the clinician to maintain sedation levels within the target range.
This may help add value to patient care by contributing to:
- Improved patient safety
- Optimised medication levels
- Reduced ventilator days
- Reduced cost
"As this technology gets better, as we have with the SedLine - easy to apply, fewer artifacts - this now becomes a functional tool to correctly control our sedation levels and reduce costs in our ICU, reduce morbidity in our ICUs and reduce stay in our ICUs."
- Michael Ramsay, MD
- Chairman
- Department of Anaesthesiology
- Baylor University Medical Center
- Dallas, TX
References
- 1.
Prichep LS, Gugino LD, John ER, et al. The Patient State Index as an indicator of the level of hypnosis under general anesthesia. Br J Anaesth. 2004,92:393-399. Available online at http://bja.oxfordjournals.org/cgi/content/full/92/3/393.
- 2.
Schneider G, Heglmeier S, Schneider J, et al. Patient State Index (PSi) measures depth of sedation in intensive care patients. Intensive Care Med. 2004,30:213-216. Abstract available online at http://www.ncbi.nlm.nih.gov/pubmed/14673519.
- 3.
Sessler CN, Grap MJ and Ramsay AE. Evaluating and monitoring analgesia and sedation in the intensive care unit. Critical Care 2008, 12(Suppl3):S2. Available online at http://ccforum.com/content/12/S3/S2.
RESOURCES
Additional Clinical Resources
- Nguyen NK, Lenkovsky F, and Joshi GP. Patient State Index during a cardiac arrest in the operating room. Anesth Analg. 2005,100:155-7. Available online at http://www.anesthesia-analgesia.org/cgi/content/full/100/1/155.
- Crippen D. Bispectral Index: Is It Ready for Prime Time in the ICU? Available online at http://www.medscape.com/viewarticle/471955. Posted March 24, 2004.
- White PF, Tang J, Ma H, et al. Is the Patient State Analyzer* with the PSArray a cost-effective alternative to the Bispectral Index Monitor during the perioperative period? Anesth Analg. 2004,99:1429-1435. Available online at http://www.anesthesia-analgesia.org/cgi/content/full/99/5/1429.
- Kurup V, Ramani R, Atanassoff PG. Sedation after spinal anesthesia in elderly patients: a preliminary observational study with the PSA-4000. Can J Anaesth. 2004 Jun-Jul;51(6):562-5. Available online at http://www.ncbi.nlm.nih.gov/pubmed/15197118.
- Schneider G, Mappes A, Neissendorfer T, Schabacker M, Kuppe H, Kochs E. EEG-based indices of anaesthesia: correlation between bispectral index and patient state index? Eur J Anaesthesiol. 2004 Jan;21(1):6-12. Available online at http://www.ncbi.nlm.nih.gov/pubmed/14768917.
- Schneider G, Gelb AW, Schmeller B, et al. Detection of awareness in surgical patients with EEG-based indices-bispectral index and patient state index. Br J Anaesth. 2003 Sep;91(3):329-35. Available online at http://bja.oxfordjournals.org/cgi/content/full/91/3/329.
- Chen X, Tang J, White PF, Wender RW, Hong M, Sloninsky A, Kariger R. A comparison of Patient State Index and Bispectral Index Values during the perioperative period. Anesth Analg. 2002;95:1669-1674. Available online at http://www.anesthesia-analgesia.org/cgi/content/full/95/6/1669.
- Hausman, L., Processed electroencephalographic changes associated with hypoglycemia during the resection of an insulinoma. Anesthesiology 2002; 97(4):1013-1014. Available online at http://journals.lww.com/anesthesiology/Fulltext/2002/10000/Processed_Electroencephalographic_Changes.40.aspx.
- Drover DR, Lemmens H, Pierce ET, Plourde G, Loyd G, Ornstein E, Prichep LS, Chabot RJ, John ER, Gugino LD. Patient State Index (PSi): Optimization of delivery and recovery from propofol, alfentenil and nitrous/oxide anesthesia. Anesthesiology. 2002; 97(1):82-89. Available online at http://journals.lww.com/anesthesiology/Fulltext/2002/07000/Patient_State_Index__Titration_of_Delivery_and.12.aspx.
- John ER, Prichep LS, Kox W, et al. Invariant Reversible QEEG Effects of Anesthetics. Conscious Cogn. 2001;10:165-183. Available online at http://www.ncbi.nlm.nih.gov/pubmed/11414713.
- Gugino LD, Chabot RJ, Prichep LS, John ER, Formanek V, Aglio LS. Quantitative EEG changes associated with loss and return of consciousness in healthy adult volunteers anesthetized with propofol or sevoflurane. Br J Anaesth. 2001;87(3):421-428. Available online at http://bja.oxfordjournals.org/cgi/content/full/87/3/421.
- Prichep LS, John ER, Gugino LD, Kox W, Chabot RJ. Quantitative EEG assessment of changes in the level of sedation/hypnosis during surgery under general anesthesia. In: Jordon C. Memory and Awareness in Anesthesia IV. London: Imperial College Press, 2000:97-107. Available online at http://www.worldscibooks.com/medsci/p190.html.